Navigating the Depths of Seasonal Affective Disorder
Seasonal Affective Disorder (SAD) is a complex mental health condition that affects millions of people worldwide, yet remains largely misunderstood by the general public. This form of depression, which is intricately linked to changes in seasons, can have profound impacts on an individual's daily life, relationships, and overall well-being. Despite its prevalence, SAD often goes undiagnosed or is dismissed as mere "winter blues." However, the reality is far more nuanced and deserving of serious attention. As we delve into the intricacies of this disorder, we'll explore its historical context, current understanding, and the innovative approaches being developed to combat its effects.

Since its initial identification, our understanding of SAD has evolved considerably. Early theories focused primarily on the role of melatonin, a hormone that regulates sleep-wake cycles and is influenced by light exposure. However, subsequent research has revealed a more complex interplay of factors, including disruptions in circadian rhythms, imbalances in neurotransmitters like serotonin, and genetic predispositions.
The Biological Mechanisms Behind SAD
At its core, SAD is believed to stem from the body’s response to reduced sunlight exposure during fall and winter months. This decrease in natural light can disrupt the body’s internal clock, or circadian rhythm, leading to a cascade of biological changes. The pineal gland, responsible for producing melatonin, becomes overactive in the absence of sufficient light, potentially causing feelings of lethargy and drowsiness.
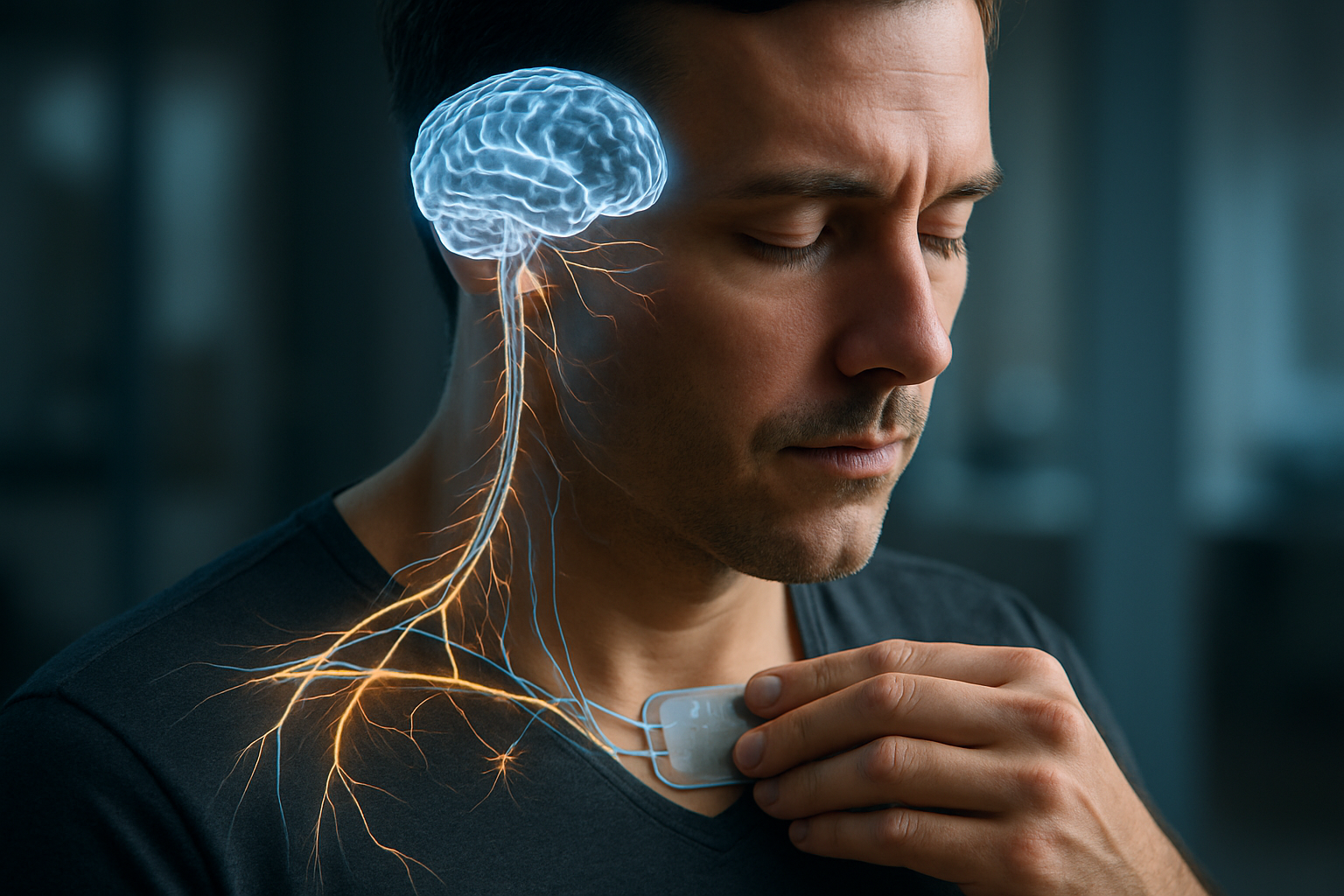
Simultaneously, the production of serotonin, often referred to as the “feel-good” neurotransmitter, may be compromised. Serotonin plays a crucial role in mood regulation, and its deficiency has been linked to depressive symptoms. Recent studies have also implicated other neurotransmitters, such as norepinephrine and dopamine, in the development of SAD, painting a picture of a complex neurochemical imbalance.
Beyond the Winter Blues: Recognizing SAD Symptoms
While SAD is commonly associated with the winter months, it’s important to note that a less common form, known as summer-pattern SAD, can occur during the spring and summer. The symptoms of SAD can vary in intensity and may include:
-
Persistent feelings of sadness or hopelessness
-
Loss of interest in previously enjoyed activities
-
Changes in appetite and weight
-
Sleep disturbances (often oversleeping in winter-pattern SAD)
-
Difficulty concentrating or making decisions
-
Social withdrawal or “hibernation”
-
Fatigue and low energy levels
These symptoms typically begin to manifest as the days grow shorter and may persist until the return of longer daylight hours in spring. The cyclical nature of SAD can make it particularly challenging for individuals to recognize and seek help, as symptoms may resolve on their own with the changing seasons.
Innovative Approaches to Treatment
The treatment landscape for SAD has expanded significantly since its initial discovery. While traditional approaches like light therapy remain cornerstone treatments, researchers and clinicians have developed a range of innovative strategies to combat the disorder.
Light therapy, which involves exposure to bright, artificial light that mimics natural sunlight, continues to be a primary intervention. However, advancements in technology have led to the development of more sophisticated light therapy devices, including dawn simulators and light boxes with adjustable color temperatures.
Cognitive-behavioral therapy (CBT) has been adapted specifically for SAD, focusing on challenging negative thought patterns associated with the changing seasons and developing coping strategies. This approach, often referred to as CBT-SAD, has shown promising results in preventing the recurrence of symptoms.
Pharmacological treatments, particularly selective serotonin reuptake inhibitors (SSRIs), have proven effective for many individuals with SAD. However, recent research has explored the potential of other medications, such as agomelatine, which targets both the serotonergic system and melatonin receptors.
The Role of Lifestyle and Environment
Emerging research suggests that lifestyle factors and environmental modifications may play a crucial role in managing SAD. Studies have shown that regular exercise, particularly when performed outdoors or in well-lit environments, can significantly alleviate symptoms. The combination of physical activity and natural light exposure appears to have a synergistic effect on mood and energy levels.
Dietary interventions have also gained attention, with some studies indicating that vitamin D supplementation may be beneficial for individuals with SAD, especially those living in northern latitudes with limited sunlight exposure. Additionally, maintaining a consistent sleep schedule and creating a bright, cheerful living environment can help mitigate the impact of reduced natural light.
Cultural and Geographical Variations
The prevalence and manifestation of SAD vary significantly across different cultures and geographical regions. While the disorder is more commonly reported in countries farther from the equator, where seasonal changes in daylight are more pronounced, it is not exclusive to these areas. Cultural factors, such as societal attitudes towards mental health and seasonal lifestyle changes, can influence both the recognition and experience of SAD.
Interestingly, some Arctic communities, despite experiencing extreme variations in daylight, report lower rates of SAD than might be expected. Researchers hypothesize that genetic adaptations and cultural practices may play a protective role in these populations, offering valuable insights for future treatment approaches.
The Future of SAD Research and Treatment
As our understanding of SAD continues to evolve, so too do the approaches to its management and treatment. Emerging areas of research include the exploration of chronotherapy, which aims to realign circadian rhythms through carefully timed light exposure and sleep schedules. Additionally, the potential of transcranial magnetic stimulation (TMS) in treating SAD is being investigated, offering a non-invasive alternative for individuals who may not respond to traditional therapies.
The integration of technology in SAD management is another promising frontier. Wearable devices that track light exposure and activity levels, coupled with smartphone apps that provide personalized recommendations, may offer individuals greater control over their symptoms and treatment plans.
In conclusion, Seasonal Affective Disorder represents a complex interplay of biological, environmental, and psychological factors. As research progresses, it becomes increasingly clear that a multifaceted approach to treatment, tailored to individual needs and circumstances, is essential. By continuing to unravel the mysteries of SAD, we move closer to more effective interventions that can significantly improve the quality of life for millions affected by this challenging disorder.